What Is the Medical Billing Process?
According to the Thirtieth European Conference on Information Systems, the transformation of medical records into the standardized diagnosis code is the process of medical billing. It is an administrative workflow mainly used in the healthcare system to manage how providers get paid for their services. It does not include medical advice, clinical decision-making, or treatment guidance. The medical billing process strictly focuses on the business and financial side of the healthcare industry.
Instead, the medical billing process focuses on:
- Ensuring smooth management of insurance claims
- Translating services into standardized codes
- Ensuring providers receive the payments for their services from insurance organizations or patients
- Coordinating financial communication between healthcare organizations and payers
Medical billing is the foundation of a healthcare organization’s revenue cycle and is essential for smooth financial functioning. The medical billing cycle ensures that every service provided is properly documented, coded, and reimbursed. It is essential for worldwide health transparency.
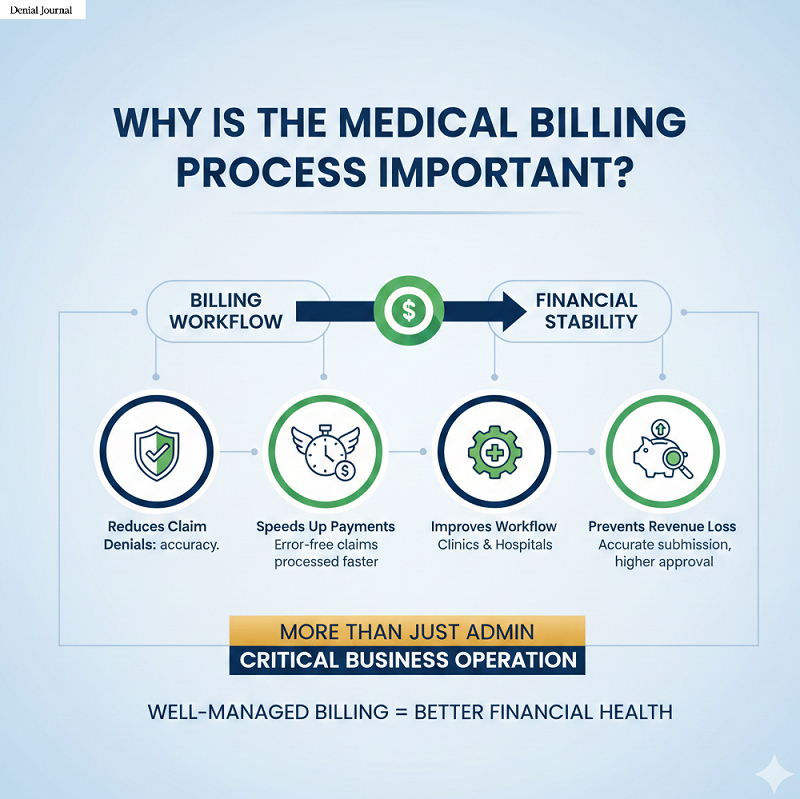
Why Is the Medical Billing Process Important?
Billing workflow has a major impact on a healthcare organization’s financial stability.
The medical billing process is important because it:
- Reduces claim denials as it ensures accuracy at each step.
- Speeds up payments from insurance companies as they process error-free claims faster.
- Improves workflow in healthcare clinics and hospitals.
- Ensures accurate claim submission and prevents revenue loss, and increases approval rates.
Medical billing is not just an administrative function but also a critical business operation. If the billing process is well managed, it leads to better financial health for any practice.
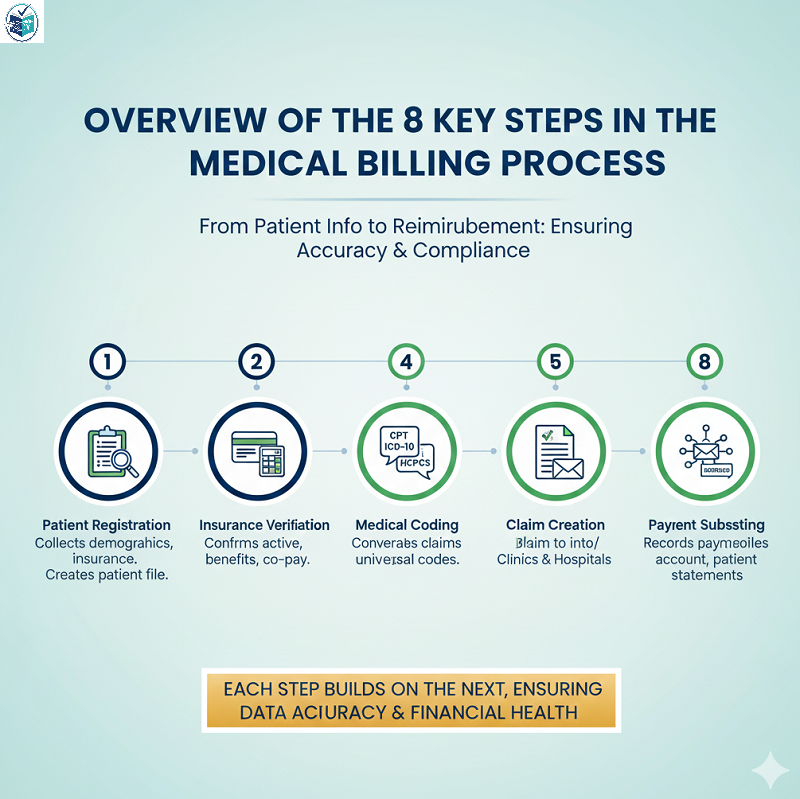
Overview of the 8 Key Steps in the Medical Billing Process
The medical billing cycle consists of eight essential steps, which begin with collecting patients’ information and their registration, and then comes the reimbursement. Each step forms the foundation of the next one, ensuring data accuracy and compliance.
1. Patient Registration
This is the first interchange in the billing workflow. During registration, the administrative staff collects:
- Patient demographic details (their name, date of birth, and address)
- Contact information
- Insurance information
- Emergency contacts
A patient file contains the mentioned details. This file is created in the system, serving as the foundation for the entire claim. Any incorrect information provided may lead to claim denials later.
2. Insurance Eligibility & Benefits Verification
Once the patient registration has been completed, billers verify:
- Whether the patient’s insurance is active
- Coverage details and limitations of the insurance
- Co-pay, deductible, and co-insurance responsibility
- Required authorizations (if applicable)
Verifying coverage early prevents claim denials and billing delays. Verification may be done through payer portals, phone calls, or integrated automated tools.
3. Medical Coding (Procedure & Diagnosis Codes)
Medical coding is a universal language that allows different computer systems to communicate with each other without ambiguity. It is the process of converting provider-documented services into required code sets.
PLEASE NOTE:
This is an educational explanation only—not diagnostic
Code sets used are:
- CPT (Current Procedural Terminology) – procedure codes
- ICD-10-CM (International Classification of Diseases)– this code tells why the patient sought medical care
- HCPCS Level II (Healthcare Common Procedure coding system) –it covers the supplies, equipment, and certain services involved
Coders ensure that documentation from the provider is translated into accurate, compliant codes. These codes describe the services performed but do not provide any medical instruction or advice.
4. Charge Entry / Charge Capture
Coded data is translated into billable charges during charge entry.
Billers:
- Enter CPT/HCPCS codes with associated fees
- Link them with the appropriate ICD-10 codes
- Review provider documentation for accuracy
Charge entry involves preparing the financial information needed to create a claim. This step builds the financial “charge slip” that becomes part of the claim later on.
5. Claim Creation (CMS-1500 / Electronic Claims)
Billers compile all verified and coded data into a formal insurance claim.
Two common formats exist for claim creation:
- CMS-1500 for professional claims
- UB-04 (CMS-1450) for institutional claims
A claim must include the following accurate details to avoid denial from insurance providers:
- Patient information
- Provider information
- Insurance details
- Codes and charges
- Dates of service
- Rendering provider identifiers (NPI, TIN)
A clean claim is one that meets all formatting, coding, and data requirements without errors and ensures clarity. Clean claims have higher rates of approval.
6. Claim Submission (To Payer or Clearinghouse)
Claim Submission is the direct process of communication between the physician practice and an insurance company.
Once the claim is completed and verified, it is submitted:
- Directly to the insurance payer
- Or through a clearinghouse, which checks for errors before forwarding
Claims are usually sent electronically through EDI (Electronic Data Interchange).
Two common EDI submission formats:
- EDI 837P (professional)
- EDI 837I (institutional)
This step is crucial because small errors can lead to rejections or delays in payments.
Submitting clean, accurate claims speeds up the reimbursement process.
7. Claim Adjudication (Insurance Review)
After submission, the payer evaluates the claim.
The payer has the right to:
- Approve the claim and issue payment
- Deny it due to errors
- Adjust it (partial approval or modification)
The payer provides an EOB (Explanation of Benefits) or ERA (Electronic Remittance Advice), which explains the payment details and adjustments, if any.
8. Payment Posting & Reconciliation
Once payment information is received, the billing team posts payments to the patient’s account and reconciles them.
Billers perform the following tasks:
- Post payments to the patient account
- Match payment amounts to expected amounts
- Identify unpaid, partially paid, or denied claims
- Send statements to patients for remaining balances
Accounts receivable (AR) teams may follow up on unpaid claims.
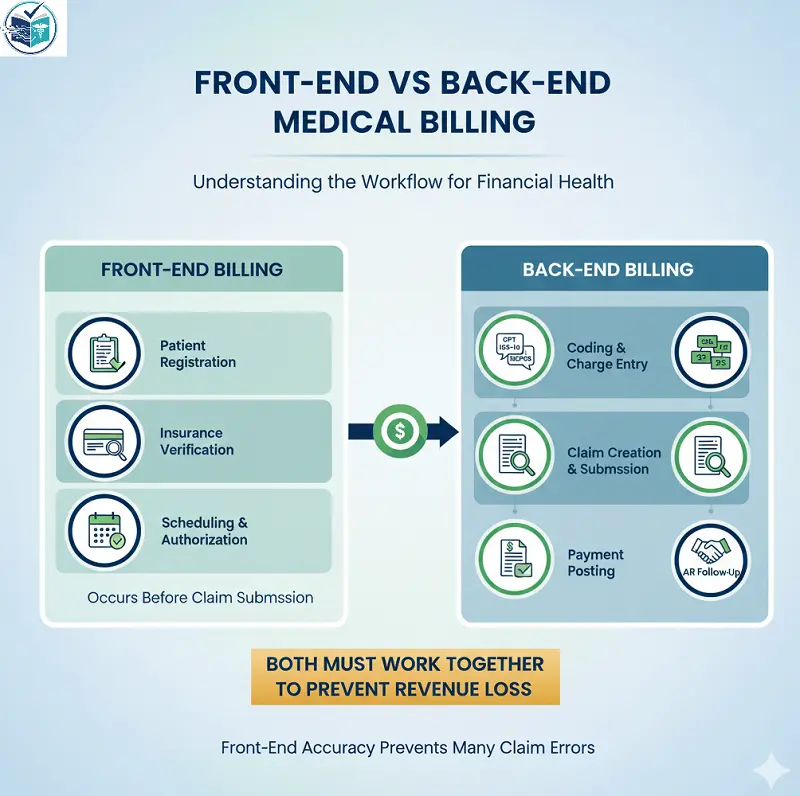
Front-End vs Back-End Medical Billing
As a beginner, let’s understand the workflow by analyzing the two sides of billing to grasp each party’s responsibilities clearly.
Front-End Billing:
Includes,
- Patient registration in medical billing
- Insurance verification
- Scheduling and authorization
These steps occur before claim submission.
Back-End Billing:
Includes,
- Coding and charge entry
- Claim creation and submission
- Adjudication review
- Payment posting and AR follow-up
Both front-end and back-end billing must work together to prevent revenue loss. Many claim errors are prevented by front-end accuracy.
Common Errors in the Medical Billing Process
A 2013 study titled Improving Hospital Billing Processes For Reducing Costs Of Billing Errors provides a detailed analysis of common errors of billing processes and how to improve those errors. Mistakes can be made by beginners or even experienced billers during this process.
Most frequent errors include:
Missing Result Error :
This error occurs when the test results are not added to the patient file or the file is missing important medical information related to the patient. If the results are missing, the bill may not be accepted.
Mismatch of Diagnosis and Tests Error:
This happens when the diagnosis of the patient and their tests don’t match.
It occurs if:
- The diagnosis is not correct.
- The diagnosis is missing.
- The diagnosis is not detailed enough or
- The tests performed do not fit the patient’s diagnosis.
Basically, the medical reason for the provider’s service and the tests do not line up.
Judicial Report Error:
This error appears in emergency cases.
The emergency department must collect proper legal documents (like police or incident reports) when needed.
If these reports are missing, the billing becomes invalid, and the claim can be processed as invalid, too.
Duplication Error:
This occurs when the same treatment or procedure is billed to a patient twice without a valid reason.
If a procedure is repeated but the doctor is unable to explain why it was repeated, it becomes a duplication error.
Material–Barcode–KIK Error:
This error happens when the hospital uses medical materials, but the proper paperwork for their usage is missing.
It can occur when:
- The invoice is missing or incorrect.
- The barcode of the material is missing.
Basically, the materials were used, but the proof or documents needed for billing are incomplete.
Preventing these errors reduces denials to some extent and improves claim approval rates.

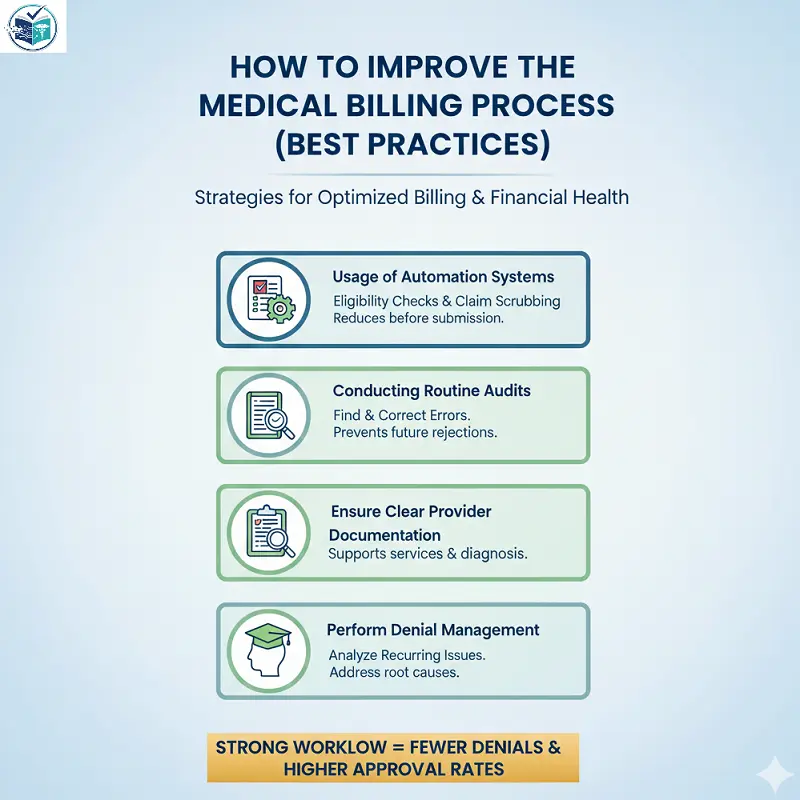
How to Improve the Medical Billing Process (Best Practices)
Healthcare organizations can optimize their billing performance by using strategies like automation tools, routine audits, clear provider documentation, and ongoing training.
A strong billing workflow includes:
- Usage of Automation systems for eligibility checks and claim scrubbing before submission
- Conducting Routine audits to find errors, if any, and correct those errors to prevent future claim rejections
- Ensure Clear provider documentation for accurate coding
- Perform Denial management procedures for analyzing recurring issues
- Provide Ongoing staff training for billing and RCM staff
These practices make billing faster, smoother, and more compliant.
Who Performs the Medical Billing Process?
The medical billing cycle is performed by the contribution of several roles.
Some roles involved in this cycle are:
- Medical billers are the ones who manage claims, posting, and AR
- Medical coders are the ones who assign CPT, ICD-10, and HCPCS codes
- RCM (Revenue Cycle Management) teams – these teams oversee payment flow
- Clearinghouses –responsible for scrubbing and forwarding claims to payers
- Insurance payers –they review and adjudicate claims
This section focuses only on job roles.

Medical Billing Process Flowchart (Text-Based)
Registration → Verification → Coding → Charge Entry → Claim Submission → Adjudication → Payment Posting → AR Follow-Up
Registration:
A patient file containing the aforementioned details is created in the system, serving as the foundation for the entire claim. Any incorrect information here may cause claim denials later. This is the first step in the medical billing process.
Verification:
Verifying coverage at an early stage prevents claim denials and billing delays. Verification may be done through payer portals, phone calls, or integrated automated tools.
Coding:
Coders ensure that documentation from the provider is translated into accurate, compliant codes. These codes describe the services performed but do not provide any medical instruction or advice.
Charge Entry:
Charge entry involves preparing the financial information needed to create a claim. This step builds the financial “charge slip” that becomes part of the claim later on.
Claim Submission:
Billers compile all verified and coded data into a formal insurance claim. A clean claim meets all formatting, coding, and data requirements without errors and ensures clarity. Clean claims have higher rates of approval.
Adjudication:
After submission, the payer evaluates the claim. The payer provides an EOB (Explanation of Benefits) or ERA (Electronic Remittance Advice), which explains the payment details and adjustments, if any.
Payment Posting:
Once payment information is received, the billing team posts payments to the patient’s account and reconciles them.
AR Follow-Up:
AR Follow-Up (Accounts Receivable Follow-Up) is the last step in the medical billing cycle, where billers track and manage all unpaid or delayed claims. The main purpose of AR Follow-Up is to make sure the healthcare provider receives the money owed by insurance companies or patients, i.e., they get paid for the services they provided.

Disclaimer:
This entire document is intended solely for educational and informational purposes. It does not provide any medical, legal, or financial advice. Healthcare organizations, billers, and readers are required to perform their own research, verify payer policies, and consult official regulatory resources before making operational decisions.
Is medical billing different from medical coding?
Yes, Coding translates services into standardized codes, while billing uses those codes to create and submit claims.
How long does the medical billing process take?
The full cycle can take anywhere from a few days to several weeks, depending on claim accuracy and payer processing time.
What is a “clean claim”?
A clean claim is one without any errors, omissions or formatting issues, and it is ready for immediate processing.
What causes claim denials?
Common reasons include inaccurate patient data, coding errors, missing authorizations, or inactive insurance coverage.
Do I need medical knowledge to understand the billing process?
No, Billing focuses on administrative and financial tasks, not on clinical work.Infact billers avoid giving any clinical advice.
What software is used in the medical billing process?
Popular tools include medical practice management (PM) systems and EHR/EMR platforms such as:
- Kareo:Kareo is a cloud-based medical billing and practice management platform. It is designed for efficient working of small to mid-sized clinics.
- AdvancedMD: AdvancedMD is a full practice management and revenue cycle management (RCM) system. It is used by larger clinics or practices with higher claim volume. It offers advanced automation features and is known for customization, robust reporting tools and it also provides strong support for multi-provider practices.
- Athenahealth : Athenahealth provides cloud-based medical billing, EHR, and practice management. It strongly focuses on automation and analytics. Its payer rules known as (AthenaRules) are continuously updated to help reduce claim denials. Many users choose Athenahealth because of its network-based model as it learns from millions of claims to improve accuracy and workflows.
- DrChrono: DrChrono is popular among small practices and specialty clinics because it supports iPad-based charting, e-prescribing and customizable clinical forms. Its billing module includes coding tools, claim submission, payment posting and built-in reporting.
Is this guide suitable for beginners?
Yes! This guide is written in simple, clear language for new billers or healthcare students.
Helpful Resources
- American Medical Association. (n.d.).
CPT® overview and code set.
https://www.ama-assn.org/practice-management/cpt - Centers for Disease Control and Prevention. (n.d.).
ICD-10-CM official guidelines and code set.
https://www.cdc.gov/nchs/icd/icd10cm.htm - Centers for Medicare & Medicaid Services. (n.d.).
Claims and billing overview.
https://www.cms.gov/Medicare/Billing - Centers for Medicare & Medicaid Services. (n.d.).
HIPAA EDI transactions and code sets.
https://www.cms.gov/Regulations-and-Guidance/Administrative-Simplification/HIPAA-EDI - Dasdemir, E., Oguz, M., Atalay, M., Bilgin, V., Testik, M., & Soydan, G. (2013, September).
Improving hospital billing processes for reducing costs of billing errors.
In Proceedings of the European Network for Business and Industrial Statistics (ENBIS) 13 Conference, Ankara, Turkey. - Derricks, J. (2021).
Overview of the claims submission, medical billing, and revenue cycle management processes.
In J. E. Szalados (Ed.), The medical-legal aspects of acute care medicine. Springer, Cham.
https://doi.org/10.1007/978-3-030-68570-6_11 - Oberste, L., Finze, N., Hoffmann, P., & Heinzl, A. (2022).
Supporting the billing process in outpatient medical care: Automated medical coding through machine learning.
In Proceedings of the European Conference on Information Systems (ECIS).

About the Author
Laim Will is a medical billing and coding content writer with 5 years of practical experience in Revenue Cycle Management (RCM). She specializes in creating beginner-friendly medical billing guides, denial management explanations, coding basics, and AR workflow insights. Her content is designed to simplify complex billing processes using real-world industry knowledge and clear explanations.